Borderline Personality Disorder Misdiagnosed as Bipolar Disorder

Borderline personality disorder is often misdiagnosed as bipolar disorder, leading to ineffective treatment and unnecessary suffering. If you believe you have been misdiagnosed, understanding the causes and prevalence of misdiagnosis as well as how to differentiate between the two illnesses can give you clarity into your own situation and help you decide whether to seek a new diagnosis and treatment.
Matthew was in pain. His mood swung through peaks and and valleys. At times his impulsivity led him to make decisions with devastating consequences. His anger, irritability, and paranoia were damaging his ability to maintain close relationships and interfering with his professional function. To his first psychiatrist, there was little mystery to Matthew’s diagnosis; he was a classic case of bipolar disorder if she ever saw one, and as he left her office, a small piece of paper with the word “Seroquel” rustled in his pocket.
To his family, identifying the source of Matthew’s distress brought the hope of restored normalcy. There was a wealth of medications available to temper the instability inherent to bipolar disorder—surely one of them would work. But although Matthew swallowed his white oblong pills dutifully, he only got worse. Within a year, he had gone through a total of three antipsychotics and two mood stabilizers, none of which alleviated his symptoms. Then, something happened—as his symptoms worsened and he began to make threats of suicide, his family implored him to seek more intensive treatment, not in the care of his normal psychiatrist, but in a residential treatment setting. There, they believed, he would be able to rapidly trial new medications and identify the pharmacology that would deliver Matthew from his pain.
Instead of discovering the perfect medications to treat Matthew’s bipolar disorder, a new psychological assessment revealed that the problem wasn’t located in the medication, but in the diagnosis itself. Matthew, like so many others, had borderline personality disorder misdiagnosed as bipolar disorder.
The Causes and Prevalence of Misdiagnosis
Misdiagnosis of mental health disorders is alarmingly common and can happen with any diagnosis. However, borderline personality disorder and bipolar disorder share common traits that lead to a particularly high rate of misdiagnosis. These include:
- Affective instability
- Irritability and anger
- Impulsivity
- Suicide attempts
- Problematic social functioning
- Psychotic experiences
This overlap of symptomatology leads to an astoundingly high prevalence of borderline personality misdiagnosed as bipolar disorder. According to a study by Camilo J. Ruggero et al. published in the Journal of Psychiatric Research, nearly 40% of people with borderline personality disorder have previously been misdiagnosed with bipolar disorder.
The causes of this high rate of misdiagnosis are multiple. First, some psychiatrists may simply not be identifying borderline personality disorder due to lack of diagnostic expertise or rigor. “One of the worst trends […] is the use of ‘symptoms checklists’ to save time in making a psychiatric diagnosis,” explains Dr. David M. Allen, professor emeritus of Psychiatry at the University of Tennessee Health Science Center. “An adequate evaluation of psychiatric symptoms must take into account their psychosocial context, their pervasiveness, and their time course.” This, of course, also relies on honest self-disclosure on the part of the client, which can be compromised by feelings of shame or lack of insight. Diagnostic bias is another major problem, spurring psychiatrists to lean toward the diagnosis they believe is more easily treatable—in this case, bipolar disorder.
Differentiating Between Borderline Personality Disorder and Bipolar Disorder
While borderline personality disorder and bipolar disorder do share symptomatology, there are important features that can help clarify diagnosis:
Duration of Mood Disturbances
People with borderline personality disorder can experience profound mood volatility, with moods shifting on a day-to-day basis, often in response to environmental factors. People with bipolar disorder, however, have prolonged episodes of mania, hypomania, and depression and do not experience the day-to-day or minute-to-minute changes so often present for people with borderline personality disorder. As Dr. Allen points out, “There is absolutely not one bit of credible scientific evidence that short-duration ‘mood swings’ are in any way related to bipolar disorder.” Additionally, while bipolar mood episodes can be prolonged, they are typically not ever-present; people with bipolar disorder can have periods of wellness lasting weeks, months, or even years while people with borderline personality disorder typically have pervasive symptoms.
Sleep Patterns
Sleep disturbances can be significant indicators of bipolar disorder. Drastically reduced need for sleep is often a hallmark of manic or hypomanic episodes whereas sleep disturbances are much less common and severe amongst people with borderline personality disorder. If sleep disturbances are present, it is essential to identify the context of those disturbances; if someone reports staying up all night it’s vital to note if their wakefulness was preceded by factors such as daytime napping or stimulant use.
Family History
Both bipolar disorder and borderline personality disorder appear to run in families. The nature of mental health disorders present within one’s family can provide important diagnostic clues.
Relationship Patterns
One of the most central features of borderline personality disorder is interpersonal conflict and the inability to maintain stable relationships. As Dr. Ken Duckworth of the National Alliance on Mental Illness says, “People with borderline personality disorder often have intense relationship histories, and many of their experiences with emotional dysregulation are in response to relationship interactions.” While bipolar disorder symptoms can interfere in relationships, relationships are not the central cause of emotional disturbance and people with bipolar disorder typically don’t experience the fundamental interpersonal volatility, fear of abandonment, and black-and-white thinking inherent to borderline personality disorder.
Self-Harm and Suicidality
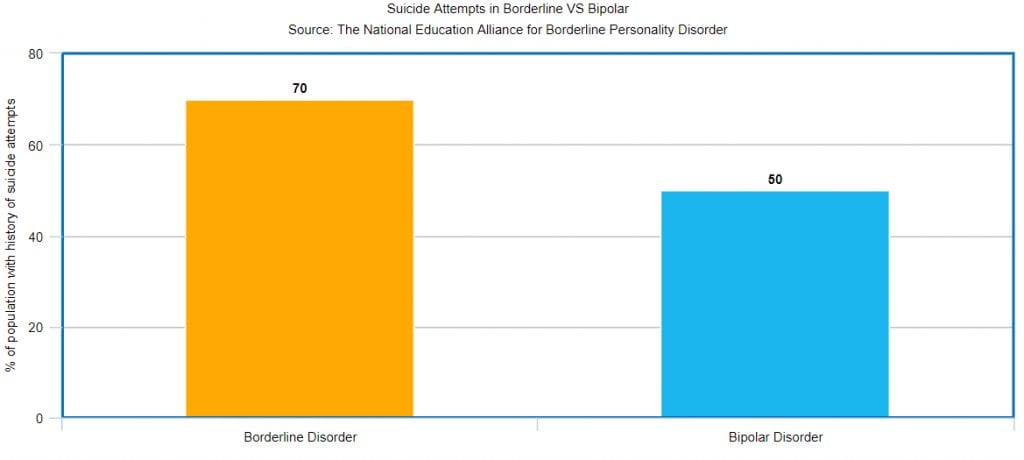
Self-harm can occur in response to a wide range of mental health disorders and the myth that self-harm automatically indicates borderline personality disorder is dangerous. However, it is true that people with borderline personality disorder are more likely to participate in self-harm than people with bipolar disorder; according to Dr. Peggy Hoffman of the National Education Alliance for Borderline Personality Disorder, self-injury such as cutting, burning, biting, and head-banging is seen in 75% of people with borderline personality. Meanwhile, 65-70% of people with borderline personality disorder attempt suicide, often repeatedly. While 50% of people with bipolar disorder also have a history of suicide attempts, they are less likely to make attempts at the rate of those with borderline personality disorder. The presence of self-harm or suicide attempts cannot be used to confirm diagnosis, examining the nature of these factors may contribute to the diagnostic process.
Psychosis
Borderline personality disorder and bipolar disorder may both feature some level of psychosis, but the specifics of these psychotic experiences are profoundly different. “People with borderline personality disorder may experience ‘micropsychotic’ phenomena of short duration (lasting hours or at most a few days), including auditory hallucinations, paranoia, and episodes of depersonalization,” says psychiatrist Dr. Bernadette Grosjean. “However, patients generally retain insight and can acknowledge that ‘something strange is happening without strong delusional thought.” In contrast, psychotic symptoms in the context of bipolar disorder are longer in duration, happen during a mood episode, and patients are often unable to identify the irrationality of their thoughts.
Borderline Personality Disorder Doesn't Have to Control Your Life
Effective BPD Treatment is Available
Seeking New Diagnosis and Treatment
Borderline personality disorder and bipolar disorder require very different kinds of treatment; while borderline personality disorder is primarily treated via psychotherapy, particularly dialectical behavior therapy (DBT), the first line of defense against bipolar disorder is medication-based. As such, when borderline personality disorder is misdiagnosed as bipolar disorder, you may be subjected to pharmacotherapies that augment your distress by introducing unpleasant side-effects and disturbing your emotional function. Just as importantly, you are denied the opportunity to begin the healing process in a way that is meaningful and effective for you, leaving you to struggle with ongoing inner pain and dysfunction.
If you suspect you have been misdiagnosed or are unsure if you have borderline personality disorder or bipolar disorder, a residential treatment environment can be an ideal place to find clarity, validation, and hope. Using a sophisticated battery of psychological assessments combined with the ongoing observation afforded by the residential environment, your clinical team can form a complete picture of your diagnosis and your overall psychological needs. With this information, they will design a customized treatment plan that addresses the full scope of your needs using cutting-edge therapies delivered by expert clinicians.
While a diagnosis of borderline personality disorder can be frightening for many, today there are more— and more effective—treatment modalities available than ever before to help you achieve emotional and behavioral stability, enhance your sense of self, and help you develop and maintain positive relationships. With the right diagnosis and the right care, you can engage in a truly transformative healing process that will allow you to realize your true potential and create inner tranquility.
Bridges to Recovery is a residential treatment center for bipolar disorder and other mental health disorders. Contact us to learn more about our renowned Los Angeles programs and how we can help you or your loved one start on the path to lasting wellness.






