Mood Disorders and Co-Occurring Eating Disorders: Why Comprehensive Treatment is Key to Recovery

If you suffer from a mood disorder and a co-occurring eating disorder, you may feel trapped in a vicious cycle from which it may seem difficult, even impossible, to escape. Understanding how nutrition impacts mood and how mood affects nutritional choices can, in turn, help you better grasp the reasons behind the comorbidity of mood and eating disorders and begin developing the tools you need to create lasting change. And, by seeking out comprehensive treatment in a residential setting which will address the root issues of both disorders, you can begin to heal and break free from the cycle at last.
Food and mood have long been known to walk hand-in-hand. What’s the stereotypical fix for feeling low? Ice cream. Chicken soup. Apple pie. There’s a reason we call it “comfort food.” But the connection runs deeper than that. Especially when it comes to mood and co-occurring eating disorders, the bidirectional link between nutrition and emotion plays a critical role in determining your overall health as well as the long-term success of your recovery efforts.
Begin Your Recovery Journey.
877-727-4343How Nutrition Impacts Mood
You may already know that mood is linked to chemicals—the phrase “I have a chemical imbalance,” for instance, has become a common casual explanation (or excuse) for irritable or depressed mood or bad behavior. And of course, nutrition is chemical, too—there’s an entire field of study dedicated to “food chemistry.” But how are the two related?
Contrary to popular belief, the mood-food connection is not quite as simple as eating a piece of chocolate to cure depression. While what you eat can affect how you feel, such quick fixes are generally low-impact and temporary. There is no one food that can “cure” a mood disorder, nor does one meal a recovery make.
What does seem to make a difference is the quality of your overall diet over an extended period of time. Recent research suggests that regular consumption of fatty, sugary foods—especially anything deep-fried or candy-coated—tends to negatively impact overall mood and mental health, while a diet consisting mainly of fruits, veggies, low-fat dairy, lean meats, and other healthier choices appears to be much more conducive to maintaining elevated moods and managing disorders and their symptoms.
In other words, eating healthy on a consistent basis is good for your mind and your body, while eating too many unhealthy foods too often can be detrimental to your mental health.
How Mood Affects Nutritional Choices
Just as food can affect how you feel, how you feel can affect what kind of dietary choices you make. “Emotional eating” is, of course, the prime example of this. You may turn to a tub of your favorite flavor of Ben & Jerry’s for consolation on a bad day, or if you’re on a diet and feeling discouraged you may give up and indulge for a day, a week, or forfeit your diet altogether. If you’re stressed out, particularly if you’re worried about an upcoming social event and craving a little “liquid courage,” you might grab a glass—or a bottle—of your liquor of choice.
A snack or a sip here and there isn’t such a big deal, nor is skipping the occasional meal when you’re in a hurry; the problem arises when the behavior becomes habitual and begins to affect your emotional stability and physical health. In much the same way that drugs cause a release of “happy” chemicals in your brain on which it’s notoriously easily to become dependent, so too do comfort foods—and they can be surprisingly addictive. This can create a vicious cycle of low mood followed by emotional eating, which then may continue or worsen the low mood, inspiring more of the unhealthy eating behavior, and so on.
While not as obvious a road to addiction as indulgent eating, severely restricting food intake can create a similar vicious cycle. Perhaps you’ve been feeling down and not getting out much, so your appetite is low. So you start skipping meals—thus beginning a potential downward spiral without even realizing it. One of the number one signs that your caloric intake is too low is a persistent lack of energy because your body isn’t getting the fuel it needs to run properly.
Comorbidity of Mood Disorders and Eating Disorders
While one doesn’t necessarily lead to the other, mood disorders and eating disorders often co-occur. According to the Psychiatric Times,
Data from epidemiologic research support the overlap between eating disorders (eg, anorexia nervosa, bulimia nervosa, binge eating disorder) and mood disorders. For example, approximately 5% of patients with MDD also have an eating disorder (all DSM-IV diagnoses); for female patients with MDD, this rate has been reported to be as high as 33%.
The rates of lifetime prevalence of mood disorders in patients with eating disorders are even higher. For anorexia nervosa, the rate is 42.1 percent; for binge eating disorder, 46.4%; and for bulimia nervosa, a whopping 70.7%. Eating disorders manifest in conjunction with a variety of mood disorders, including both anxiety and depressive disorders as well as bipolar, dysthymia, and more.
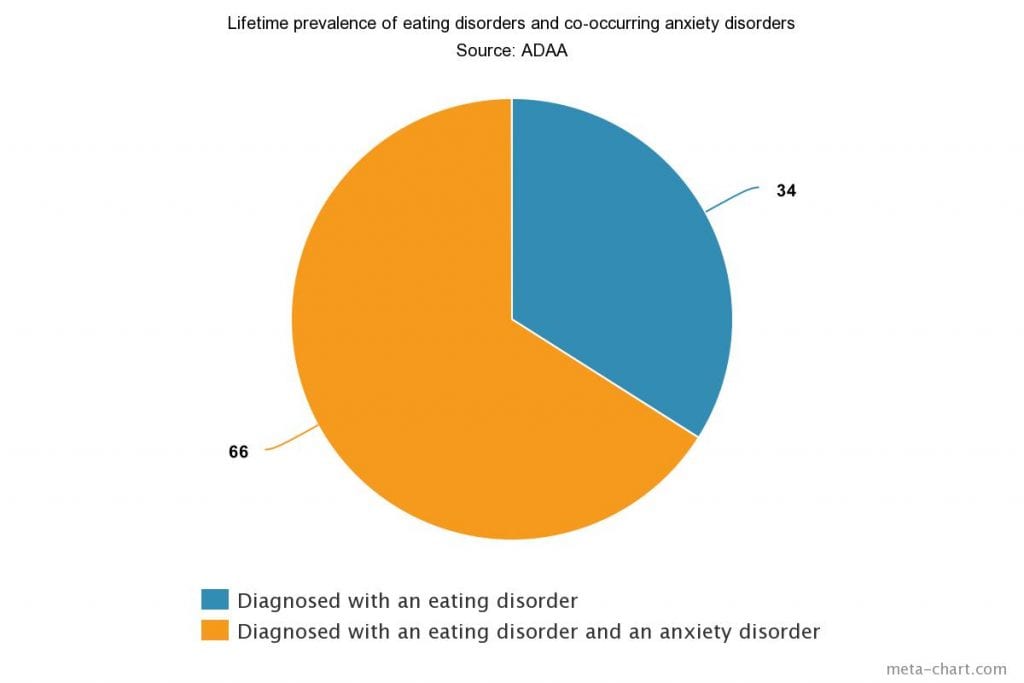
Furthermore, according to the Anxiety and Depression Association of America (ADAA), “two-thirds of people with eating disorders suffer from an anxiety disorder at some point in their lives and that around 42 percent had developed an anxiety disorder during childhood, well before the onset of their eating disorder.”
The most common anxiety disorder to co-occur with an eating disorder is obsessive-compulsive disorder (OCD). In addition to the major overlapping factors of food and mood discussed above, those who suffer from both OCD and an eating disorder may experience unique symptoms which create further overlap between the two, such as obsessive thinking about food or weight, compulsions like dividing food into tiny, precisely measured portions, or binge eating.
Call for a Free Confidential Assessment.
877-727-4343Comprehensive Treatment for Mood Disorders and Co-Occurring Eating Disorders
Because mood and eating disorders are so closely linked, successful treatment of either is highly dependent on a comprehensive program which addresses the roots of both. Attempting to only treat the mood disorder may not relieve the symptoms of the eating disorder, which can then trigger relapse of the mood disorder (due to continued weight gain, for example, or perceived lack of weight loss) down the road. Similarly, attempting to only treat an eating disorder without taking into account the anxieties or depressive symptoms which may have directly contributed to its onset in the first place once again creates a high risk of future relapse.
Cognitive Behavioral Therapy (CBT) has been shown to be especially helpful when treating co-occurring mood and eating disorders, as it focuses on altering the thoughts and behavioral patterns which contribute to both depression/anxiety and emotional eating by replacing them with new, healthier habits and perceptions. A good comprehensive treatment program will combine CBT with a balanced diet plan crafted with the help of an expert nutritionist, as well as medical prescriptions (if appropriate) to alleviate symptoms, in order to create an effective and sustainable path to recovery. And, in a residential setting, you’ll have the medical and personal support you need to focus on getting well without the distractions of everyday stresses and temptations—and time enough to heal at a pace that’s right for you.
Bridges to Recovery offers comprehensive residential treatment for people struggling with mood disorders as well as co-occurring substance abuse and eating disorders. Contact us to learn more about our renowned Los Angeles programs, and how we can help you or your loved one start on the path to lasting wellness.






